Curriculum
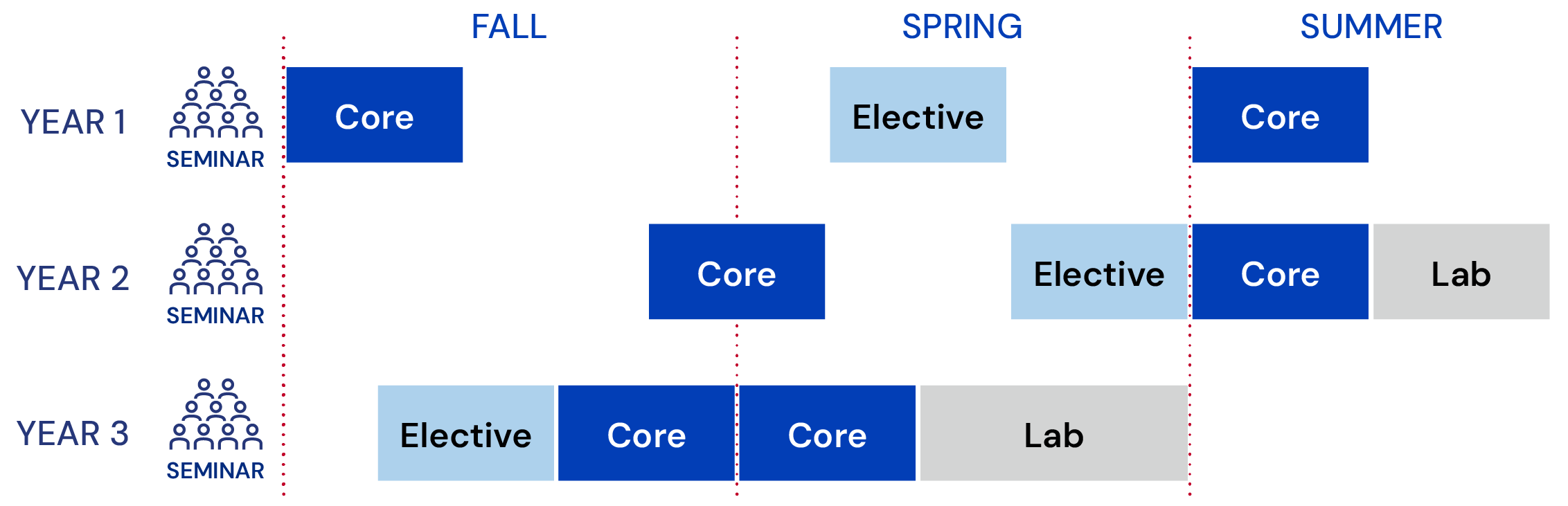
The curriculum for Penn’s Master of Health Care Innovation online program helps students develop multidisciplinary foundations for critical, analytic thinking about health care solutions. Core courses build a common foundation. Electives explore special subjects. Labs encourage practicing innovation methods. And throughout, students build their network while learning with and from their cohort.
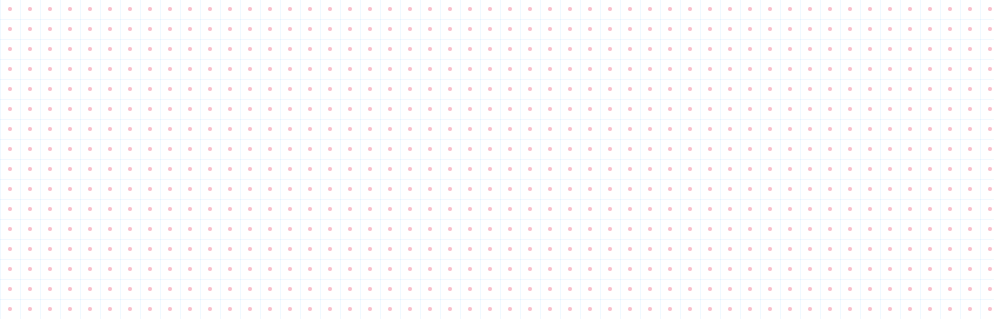
The Master of Health Care Innovation program is designed to be completed in 20 months. Students take one course at a time, with one week off between courses as a brief pause in the program's intense pace. Extended breaks occur over the winter holidays and summer. A flexible 3-year option is available for students who prefer to stretch the workload and financial commitment over more time.
Students are required to complete 11 course units (CU) to earn the degree. (At Penn, 1 course unit is usually converted to a 4-semester-hour course.) For the Master of Health Care Innovation, a 1.0 CU course is intentionally designed as 6 rigorous weeks of learning and interacting. Students typically spend 12–15 hours per week on coursework. Most activity is asynchronous, offering flexibility that is paired with predictable weekly deadlines to structure your time.
The curriculum consists of:
- 6 core courses (6.0 CU)
- 3 electives (3.0 CU)
- 2 lab courses (2.0 CU)
In addition, students attend the MHCI Seminar each August in person on Penn's campus in Philadelphia (public health measures allowing). Seminar is required, although it does not confer course credit.
MHCI students may also participate in extracurricular opportunities, such as attending virtual talks or programs from the Leonard Davis Institute of Health Economics and Penn Health-Tech.
Penn’s MHCI program is committed to maintaining a leading, competitive position at the intersection of health care and online education as health care transforms, society shifts, and the program grows. To accomplish this we regularly conduct interviews with leaders from across health care to identify emerging trends, recent gaps, and expectations for MHCI alumni. We also listen to our students, alumni, and Curriculum Committee for input so we can design and deliver an exceptional learning experience with real-world impact.
A revised curriculum launched in Fall 2022. Key changes included:
- Health Equity is becoming a required 1.0 CU course, as well as a topic addressed across the curriculum.
- An additional elective slot provides greater flexibility for students to explore special topics, such as digital health, AI, and data.
- Key topics--e.g. patient-centric care, behavioral health, telemedicine--are addressed in multiple courses across the curriculum.
- Labs are extended to 1.0 CU each, allowing more time to address challenges and develop skills to pitch innovation.
- Many courses will include a final deliverable to create an innovation portfolio to showcase your thinking, innovation, and leadership skills.
Every year all individual MHCI courses are reviewed by faculty and the MEHP Online instructional team. They update course material and activities as needed to create the most effective learning experience.
Standard Track (20 months)
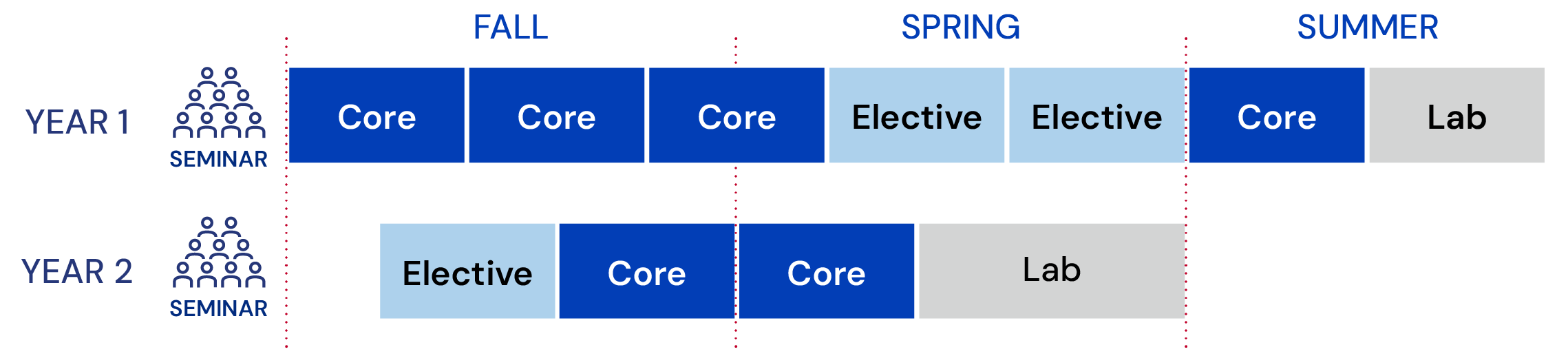
Students who choose the extended 3-year track must meet the same degree requirements as the 20-month program. The first year's coursework is distributed across 2 years, and the final year's schedule remains the same. If you choose this program option, an advisor will help you identify the best schedule.
Extended Track (3 years, lighter start)
Master of Health Care Innovation core and elective courses are designed with a similar structure to enhance learning new knowledge, skills, and practices. The primary course activities include:
- Engaging with content and media — Brief, high-quality video lectures; interview cases; cutting-edge readings; and learning aids, many of them downloadable, are predictably structured in weekly modules for you to study on your own schedule.
- Interacting with classmates, faculty, and the course team — During live class meetings and asynchronous class time, you will synthesize knowledge, explore scenarios and cases, identify opportunities for innovation, and network with colleagues.
- Applying your learning — Practice activities, ongoing projects, and presentations help you hone your ideas, identify stakeholders and decision makers, develop strategies for persuasion and negotiation, and strengthen your arguments in a safe, supportive space. You will collect special assignments across several courses into an Innovation Portfolio to showcase your innovation work.
Download full listing of 2025-2026 courses by core and elective with faculty and a short description.
Students are required to attend the annual MHCI Seminar. Occurring in August, it provides an orientation to the upcoming schoolyear, immerses students in innovation topics, and builds connections between students, the program, and Penn.
Standard components include:
- Program and classroom orientations
- Panel discussions
- Faculty presentations
- Interactive workshops to develop professional skills
- Social events
- Networking activities